What You Need to Know About Prostate Cancer
The Prostate
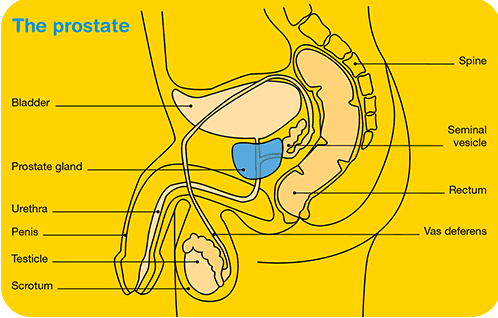
The prostate is a small walnut sized gland institute only in men. It sits simply below the float and surrounds the urethra, the tube which carries urine and ejaculate along the length of the penis and to the exterior of the torso Its function is to produce function of the fluid that makes up semen. The male hormone testosterone, which is produced mainly past the testicles, has a key role in controlling prostate growth and development. Every bit men age the prostate tends to increment in size, which can cause urinary problems and symptoms associated with prostatitis or beneficial prostatic hyperplasia (BPH) which is non-malignant.
What is Prostate Cancer?
Prostate Cancer results from the growth of abnormal cells within the glands of the prostate. These glands are lined with cells that secrete the protein prostate specific antigen (PSA). The cancerous overgrowth can occur in these secretory cells.
Source: http://www.cancer.org.au/
Staging
The staging of prostate cancer is determined by the extent to which the cancer has been contained inside the prostate or has spread to other parts of the body:
Localised prostate cancer – the cancer has non grown beyond the prostate.
Locally advanced prostate cancer – the cancer has spread exterior the prostate to nearby organs and tissues, but still remains within the prostate region.
Metastatic prostate cancer – the cancer has spread to other parts of the body like the lymph nodes or basic.
The TNM Arrangement is the most widely used method for staging and grading prostate cancer:
T (Tumour) Stage: shows if a tumour has spread outside the prostate or the region. Physical Digital Rectal Examination (DRE), imaging, biopsy, or endoscopy help with T staging.
Northward (Node) Stage: shows if a tumour has spread to lymph nodes in the pelvic regions. This is typically assessed by imaging and a transrectal ultrasound during prostate biopsy.
M (Metastatic) Stage: shows if a tumour had spread to other sites such as the bones. This is typically assessed by imaging such as a whole trunk bone browse.

Source: http://www.cancer.org.au/
What are the Adventure Factors for Prostate Cancer?
The main established take chances factors are age, family unit history and race/ethnicity:
Age
- The older you are the more than probable you are to develop prostate cancer. Males under fifty are rarely diagnosed, simply the take chances of diagnosis by the age of 75 years is 1 in viii in 2013.
Family History
- If you have had a kickoff-degree relative (male parent, brother or son) with prostate cancer, and so you accept a higher hazard of developing it, peculiarly if they were diagnosed at an earlier age. For example, if your male parent was diagnosed at age 50, then your risk of developing prostate cancer is doubled. If you take had two relatives diagnosed at 50 years, then your run a risk is up to seven times higher.
Race/Ethnicity
- Prostate cancer diagnoses vary between ethnic groups. For example, males with an African groundwork have a higher risk, compared with males with an Asian/Pacific Islander groundwork.
Other possible risk factors that could have an consequence on prostate cancer:
Genetics
- Mutations in the BRCA1 and BRCA2 genes may enhance the likelihood of prostate cancer risk. Men who know they have these mutations may consider screening at an before historic period.
Nutrition
- Whilst there is no direct proof, some studies propose that eating a lot of saturated fatty in your diet may increment your chances of prostate cancer. WebMD provides a listing of recommended items to help with a prostate cancer nutrition.
Alcohol
- Some studies have suggested that drinking may increase the hazard of prostate cancer. A recent meta-analysis suggested that six drinks or more per day can increase your hazard of developing prostate cancer past 18% compared with men who exercise not potable.
How is Prostate Cancer Detected and Diagnosed?
The near common tests are:
Digital Rectal Examination (DRE) – If your md is testing for prostate cancer, they may want to do a physical exam to determine if the prostate feels hard or bumpy.
PSA Test – The Prostate-Specific Antigen (PSA) claret test is a screening tool for early detection of prostate cancer. It measures the level of prostate specific antigen in the blood, which is produced past the prostate gland. PSA levels in the blood naturally increase with increasing age. College levels than normal are a possible indicator for prostate cancer. PSA levels can also rise due to benign prostatic enlargement, inflammation or infection. Every bit a cancer screening tool, the exam is non perfect, with high numbers of false positive and some false negatives.
Prostate Biopsy – Under ultrasound guidance a biopsy needle is inserted into the prostate by a Urologist and a core or sample is removed to determine if any cancer cells are present. This is the only manner to provide a definitive diagnosis of prostate cancer. When examined under the microscope a pathologist volition report the number of positive and/or negative cores, as well equally the Gleason Grade if positive for cancer.
Magnetic Resonance Imaging (MRI) – An MRI may indicate evidence of cancer in the prostate gland, particularly if y'all have a high or rising prostate-specific antigen (PSA) level.
How Common is Prostate Cancer in Australia?
Diagnosis
- Estimated eighteen,223 new cases diagnosed in 2020
- About common diagnosed cancer in males
Incidence
- 1 in every 8 males aged to 75 years has prostate cancer
Age
- Median historic period at diagnosis is 67.half-dozen years
Treatment
Radiotherapy
- 26% of males (one quarter of all men who had a radiotherapy grade in 2014-15) were for prostate cancer
Survival
- 95 % of men with prostate cancer survive for at least 5 years following diagnosis compared to other males with commonly diagnosed cancers
- At the terminate of 2012, 94,114 males diagnosed with prostate cancer in the previous five years were nevertheless alive
- seven% of men had survived 15 years later diagnosis (2009-2013)
Deaths
- 1 in every 130 males aged to 75 years dies from prostate cancer
- Prostate cancer is the second virtually common cause of cancer death in males
- 4% of all male deaths in 2019 were from prostate cancer
- iii,376 deaths from prostate cancer are estimated in 2020
Brunt of Disease
- Prostate cancer is the third almost common cancer in males (10%) that contributes to Australia'south cancer burden in 2011
Aboriginal and Torres Strait Islander People
- Indigenous Australians are 20% less probable to dice from prostate cancer than non-indigenous Australians
Remoteness Expanse
- Men living in inner regional areas were i.five times more than likely to be diagnosed with prostate cancer than those living in very remote areas (2008-2012)
- Men living in very remote areas are 1.2 times more than likely to dice from prostate cancer than those from major cities (2010-2014)
Socioeconomic group
- Men in the lowest socioeconomic group were 1.ii times more probable to dice from prostate cancer than compared with the highest group
What are the Signs and Symptoms of Prostate Cancer?
In the early stages, prostate cancer may cause no signs or symptoms at all. As a tedious-growing cancer information technology may non show any obvious symptoms for years.
But with many men over l years the symptoms of prostate cancer tin include:
- The demand to frequently urinate, by and large at night
- A sudden need to urinate
- Difficulty and pain when starting to urinate
- Burning sensation or pain during urination
- Leakage afterwards urination
- Incomplete elimination of the float
- A weak, dribbling flow of urine
- Difficulty in getting an erection (erectile dysfunction)
- Painful ejaculation or a subtract in the corporeality of fluid that is ejaculated
- Blood in the urine (haematuria) or semen
More generally, symptoms can range from:
- Pain and stiffness in the basic, lower back, pelvis, sciatica, and thighs
- Swelling in the legs or pelvic region
- Numbness or pain in the feet, legs or hips
- Unexplained weight loss and fatigue
What is the Treatment for Prostate Cancer?
Prostate cancer is a ho-hum growing illness, and in nigh cases men volition have time to make a decision about the best type of treatment that is suited to them. Talking almost treatment options with your physician based on your personal diagnosis will help you brand an informed determination, specially weighing up the advantages and disadvantages, possible side effects similar incontinence and infertility, availability and cost. In full general the handling options are:

Source: http://www.cancer.org.au/
1. No Treatment
Active Surveillance
Active Surveillance is for close monitoring of low risk biopsy-diagnosed prostate cancer. This tin involve regular PSA testing, biopsies (every 1- 3 years), MRI scans and check-ups for maintenance of quality of life, or until intervention is necessary.
Watchful Waiting
This choice is for observing prostate cancer, a less intensive form of active surveillance that requires fewer tests and no biopsies.
ii. Radiotherapy
Radiotherapy is offered to men with localised prostate cancer with the intent to cure. The main two types are:
Brachytherapy
Low dose rate (LDR) using permanent radioactive seeds or high dose rate (HDR) using temporary seeds targeted direct to the prostate.
External Beam Radiation Therapy (EBRT)
EBRT involves radiotherapy applied outside the body. It uses loftier energy x-ray beams directed towards the prostate daily over a flow of seven weeks.
3. Surgery
Radical Prostatectomy
This option is the surgical removal of the prostate gland, part of the urethra and seminal vesicles. Radical prostatectomy tin can be performed laparoscopically, Robot Assisted or as an Open (small cut through the lower abdomen). Information technology normally requires a few days in hospital and your usual activities can be resumed after several weeks. At that place are some possible side furnishings to surgery to discuss with your md: nerve impairment, loss of bladder control, erectile dysfunction and infertility.
4. Hormones
Androgen Deprivation Therapy (ADT)
Reducing hormones to slow the growth of prostate cancer is a mutual handling for men with advanced prostate cancer. Hormone therapy reduces testosterone levels in the promise of slowing cancer growth or keeping it under command.
5. Chemotherapy
May exist offered if other forms of treatment take not been effective.
Sources
- Australian Cancer Network and Australian Prostate Cancer Collaboration. Guidelines for Localised Prostate Cancer: A Guide For Men and Their Families. Quaternary Edition October 2010.
- Australian Establish of Health and Welfare & Australasian Association of Cancer Registries 2017. Cancer in Australia: in brief 2017. Cancer serial no. 102. Cat.no. Can 101. Canberra: AIHW
- Australian Constitute of Health and Welfare (AIHW) 2017. Australian Cancer Incidence and Mortality (ACIM) books: " & B10 & ". Canberra: AIHW. http:// world wide web.aihw.gov.au/acim-books/
- Australian Institute of Health and Welfare 2013. Prostate cancer in Commonwealth of australia. Cancer series no. 79. Cat. no. Can 76. Canberra: AIHW.
- Cancer Treatment Centers of America . 2017.Prostate cancer symptoms. [ONLINE] Bachelor at: http://www.cancercenter.com/prostate-cancer/symptoms/. [Accessed xiv February 2017]
- Prostate Cancer Foundation of Australia. 2017.What you demand to know nigh prostate cancer. [ONLINE] Available at: http://www.prostate.org.au/awareness/full general-information/what-you-need-to-know-well-nigh-prostate-cancer . [Accessed 1 February 2017]
- Cancer Quango Commonwealth of australia. 2017.Prostate Cancer. [ONLINE] Bachelor at: http://www.cancer.org.au/about-cancer/types-of-cancer/prostate-cancer.html . [Accessed 2 February 2017]
- Australian Institute of Health and Welfare. 2017.Cancer. [ONLINE] Available at: http://www.aihw.gov.au/cancer/. [Accessed fourteen Feb 2017]
- Cancer Council Commonwealth of australia. April 2016. Understanding Prostate Cancer: A guide for people with cancer, their families and friends. [ONLINE] Bachelor at: http://www.cancer.org.au/content/about_cancer/ebooks/cancertypes/Understanding_Prostate_cancer_booklet_April_2016.pdf#_ga=1.265333641.70264329.1468204414 [Accessed fourteen February 2017]
- Cancer Council Australia. 2017.Link betwixt smoking and cancer. [ONLINE] Available at: http://wiki.cancer.org.au/policy/Tobacco_control/Link_between_smoking_and_cancer. [Accessed 14 February 2017]
- Centers of Disease Control and Prevention. 2017. Prostate Cancer Rates by Race and Ethnicity. [ONLINE] Available at: https://www.cdc.gov/cancer/prostate/statistics/race.htm. [Accessed 14 February 2017]
- Zhao J, Stockwell T, Roemer A, Chikritzhs T. Is alcohol consumption a risk factor for prostate cancer? A systematic review and meta–analysis. DOI: 10.1186/s12885-016-2891-z BMC Cancer. 2016; 16(ane):845.
-
- Australian Family unit Physician. 2017.Active Surveillance equally a Direction Option. [ONLINE] Bachelor at: http://www.racgp.org.au/download/Documents/AFP/2013/Jan/February/201301yaxley.pdf. [Accessed 14 February 2017]
- Australian Family unit Physician. 2017.Active Surveillance equally a Direction Option. [ONLINE] Bachelor at: http://www.racgp.org.au/download/Documents/AFP/2013/Jan/February/201301yaxley.pdf. [Accessed 14 February 2017]
- Gann, P. H. (2002). Risk Factors for Prostate Cancer.Reviews in Urology,4(Suppl 5), S3–S10.
- WebMD. 2017. Is There a Prostate Cancer Nutrition?. [ONLINE] Available at: http://www.webmd.com/prostate-cancer/features/is-there-prostate-cancer-diet. [Accessed twenty February 2017].
This folio was last updated on: 29 May 2017
Source: https://www.prostatehealth.org.au/about-prostate-cancer/everything-need-know-prostate-cancer/
Belum ada Komentar untuk "What You Need to Know About Prostate Cancer"
Posting Komentar